Spine Anatomy
The spine is a repeating sequence of vertebral bones, separated by discs in the front of the spine and a pair of facet joints in the back of the spine. The discs provide shock absorption between the vertebral bones and allow spine motion. Because the discs are located in the front of the spine, disc pain classically worsens while sitting and improves while standing. Disc pain can be felt in the low back or can refer pain in the buttock region and even into the back of the thighs. This referred disc pain can be felt on one side or both. The typical evolution of disc pain over time is that the flare-up episodes occur more frequently, last longer, and the associated pain becomes more intense. Eventually, the situation can progress to constant daily lumbar (low back) disc pain with superimposed flare-ups. This process often interferes with activities, erodes the quality of life, causes frustration, and often leads to desperation.
How Disc Abnormalities Occur
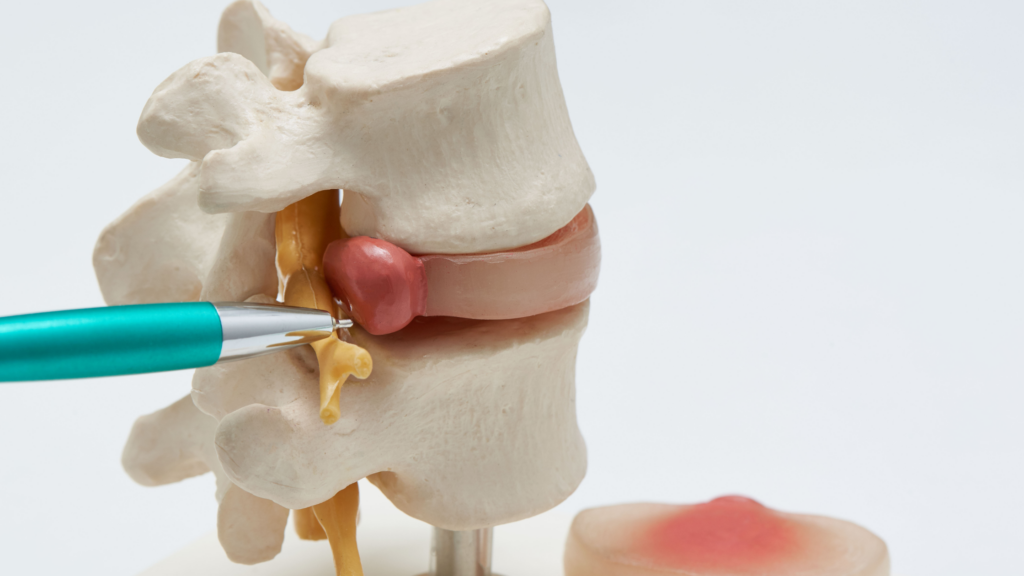
The center of the disc is called the nucleus pulposus and has a gel-like consistency. The disc’s outer ring is called the annulus fibrosus and has a sturdier but still flexible structure. Due to injury or degeneration, cracks (fissures) develop in the discs from the inside out. These cracks are called fissures and often correlate on an MRI with a high-intensity zone (HIZ) visible in the disc annulus. Sometimes MRI reports call these disc abnormalities “annular fissures” or “annular rents .” Because the disc lacks an adequate blood supply, these disc annulus fissures cannot heal spontaneously. As a result, disc annulus fissures extend in length and become more numerous with additional branching complexity over time. The discs themselves can become painful because of this process.
The Difference Between a Disc Bulge and Disc Protrusion
As more disc fissures form and progress, the disc annulus is weakened, causing it to be displaced beyond its typical boundaries. If the disc annulus displacement involves less than 90 degrees (<25%) of the disc circumference, then it is called a disc PROTRUSION; however, if the disc displacement involves greater than 90 degrees (>25%) of the disc circumference, then it is called a disc BULGE. The distinction between these terms depends on how much the disc wall is displaced. Therefore, a disc protrusion may not feel different from a disc bulge. An effort is being made for all Radiologists (doctors who specialize in interpreting MRIs, x-rays, etc.) to use standardized vocabulary in their MRI reports, especially when it comes to spine MRIs. The difference between a protrusion and a bulge allows the Radiologist to communicate how much of the disc is involved. Although these two terms are sometimes used interchangeably, they have different meanings regarding how discs appear on an MRI, even though they may not feel different to a person who has a disc abnormality. Terms like “slipped disc” and “ruptured disc” are being purposefully avoided.
For a disc protrusion or a disc bulge to be present, disc annulus fissures must be present to cause the weakening of the disc wall. When disc annulus fissures extend long enough to travel through the entire thickness of the disc annulus, then specific molecules can leak out of the center of the disc (nucleus pulposus), through the disc annulus fissures and into the epidural space, which is where spinal nerves are located. These leaking molecules trigger a series of chemical reactions that result in inflammation, which is irritating to nerve tissue. This inflammatory process can cause nerve pain symptoms in the corresponding leg even without any MRI evidence of a compressed “pinched” nerve.
Disc fissures will never repair on their own because the disc lacks a blood supply sufficient for healing. Because of the same lack of blood supply, disc fissures cannot be surgically sewn successfully. If left untreated, disc fissures predictably progress and eventually reach the outermost portion of the disc annulus, causing them to leak over time. The center of the disc (nucleus pulposus) eventually loses enough of its fluid content causing the disc to decrease in height and eventually collapse. This process is called Degenerative Disc Disease. On MRI, these discs appear dark and flat compared to discs that are not degenerating.
Learn About Discseel®
The only way to solve this problem is to seal the disc fissures, ideally before the disc starts to collapse. Because this cannot be accomplished surgically, an ideal non-surgical alternative is Discseel®. This new non-surgical procedure injects the healing protein fibrin into each tear to immediately seal the disc. Over the following months, the fibrin promotes disc tissue growth, sealing and healing previously torn discs. Several other injection procedures attempt to treat disc pain (stem cells, PRP, etc.), but they are all limited by the fact that they cannot immediately seal the disc tears, and these products end up leaking back out of the disc, which minimizes their benefit. Learn more about Discseel® at RegenerativeSpineAndJoint.com and discover how your low back disc protrusions and bulges can be successfully treated non-surgically.
Fill out the form below to learn more about the difference between a disc bulge and disc protrusion.