Magnetic Resonance Imaging (MRI) is the gold standard for detecting lumbar disc abnormalities, including protrusions, bulges, herniations, extrusions, and degenerative disc disease (DDD). Its superior ability to visualize soft tissues without exposure to radiation has made it indispensable in spinal diagnostics. However, while MRI is highly sensitive, it is not without limitations, especially in detecting subtle annulus fissures.
Sensitivity of MRI in Detecting Lumbar Disc Abnormalities
1. Disc Protrusions and Bulges: MRI is exceptionally sensitive in detecting disc protrusions and bulges, which are common causes of lower back pain. Disc protrusions occur when the nucleus pulposus, the gel-like core of the disc, pushes against the outer annulus fibrosus without fully breaching it. This condition often appears on MRI as a localized outpouching of the disc beyond its normal boundaries. Disc bulges, which are more generalized extensions of the disc material, involve a broader area of the disc circumference.
T2-weighted MRI sequences are particularly useful for visualizing these conditions. The high contrast between the hydrated nucleus pulposus and the surrounding annulus fibrosus allows for precise identification of disc contour abnormalities. MRI’s sensitivity in this context is crucial for determining whether the protrusion or bulge is impinging on adjacent nerve roots or narrowing the spinal canal, which can cause symptoms.
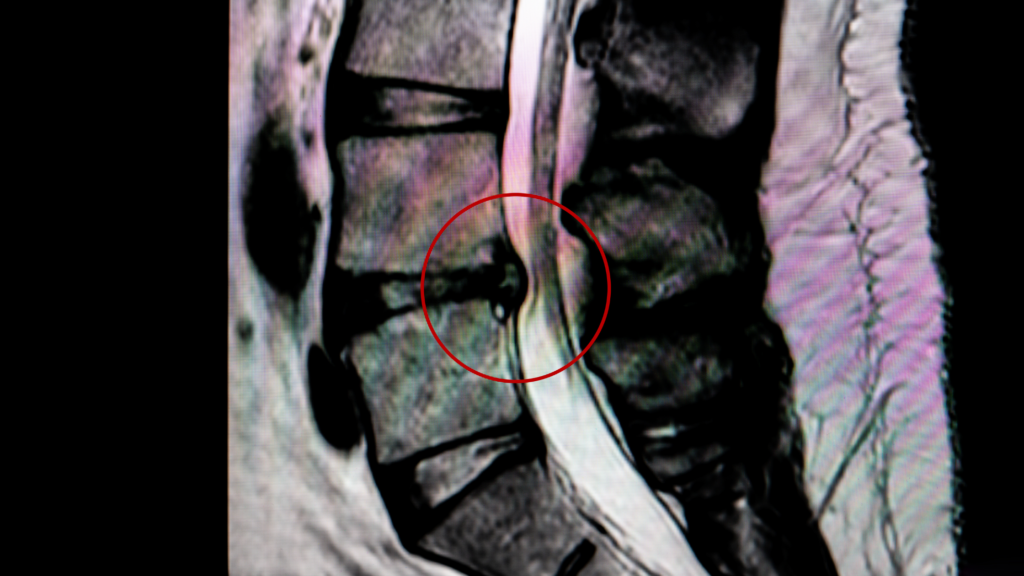
2. Disc Herniations and Extrusions: Herniations represent a more advanced stage of disc degeneration, where the nucleus pulposus breaches the annulus fibrosus, potentially causing nerve compression. MRI is highly sensitive to herniations, as it provides detailed images that reveal the extent and exact location of the herniated material. Herniations are often categorized based on their severity and location, with extrusions being a more severe form, where the nucleus material extends beyond the disc space and potentially into the epidural space.
Sagittal and axial MRI images are particularly effective in showing the relationship between the herniated disc material and the neural elements, including the spinal cord and nerve roots. This capability is essential for planning treatment, whether surgical or conservative.
3. Degenerative Disc Disease (DDD): Degenerative Disc Disease is characterized by the gradual breakdown of the intervertebral discs, often leading to reduced disc height, disc dehydration, and changes in the adjacent vertebrae. MRI is particularly sensitive in detecting these changes, especially through T2-weighted images, where dehydrated discs appear with reduced signal intensity. These images also help identify other features of DDD, such as disc space narrowing, annular tears, and Modic changes, which indicate bone marrow alterations adjacent to the degenerating disc.
High-Intensity Zones (HIZ) and Annulus Fissures
One of the most significant features on MRI that correlates with annular fissures is the presence of high-intensity zones (HIZ). HIZs appear as localized areas of increased signal intensity within the annulus fibrosus on T2-weighted images. These zones are typically associated with tears or fissures in the annulus fibrosus, which allow fluid to accumulate within the fissure, leading to the characteristic high-intensity appearance on MRI.
The presence of HIZs is often considered a marker of discogenic pain, as annular fissures are thought to expose nociceptive nerve fibers in the outer annulus to the internal disc material, which can trigger pain. However, not all annular fissures manifest as HIZs on MRI. There are several reasons for this:
- Fluid Content: HIZs are most visible when there is a sufficient amount of fluid within the fissure. If the fissure is dry or if it contains only a small amount of fluid, it may not produce the high signal intensity required to be detected as an HIZ on MRI.
- Size and Location of the Fissure: Small or peripheral annular fissures may not be large enough to create a detectable HIZ. Additionally, fissures that do not extend into the posterior annulus, where most HIZs are typically found, may be missed on MRI.
- MRI Resolution: The sensitivity of MRI in detecting annular fissures also depends on the resolution of the imaging equipment. Higher-field MRI machines (e.g., 3 Tesla) provide better resolution, increasing the likelihood of detecting small or subtle HIZs. However, even with high-resolution imaging, some fissures may still go undetected.
- Subtle Fissures: Early or micro-fissures within the annulus fibrosus might be too small to produce a detectable HIZ on standard MRI scans. These fissures may only become visible as they progress or if they accumulate more fluid over time.
Conclusion
MRI is a powerful and sensitive tool for detecting a wide range of lumbar disc abnormalities, including protrusions, bulges, herniations, extrusions, and degenerative disc disease. The appearance of high-intensity zones on MRI is particularly significant for identifying annular fissures, which are closely associated with discogenic pain. However, not all annular fissures are visible on MRI due to factors such as the amount of fluid in the fissure, its size and location, and the resolution of the imaging equipment. Understanding these nuances is crucial for accurate diagnosis and treatment planning in patients with lumbar spine disorders. Combining a lumbar MRI with an annulogram is an excellent means of fully understanding disc related lumbar pain when Discseel is being considered as a nonsurgical treatment intervention.
Contact Regenerative Spine and Joint Center to learn more.